Medical Research Council (MRC) Dyspnea Scale
STUDY MATERIAL
PhysioAlchemy
7/30/2025
The Medical Research Council (MRC) Dyspnea Scale is a simple and widely used tool to assess the level of breathlessness experienced by a patient during daily physical activity. It’s most often used for patients with chronic respiratory diseases like COPD (Chronic Obstructive Pulmonary Disease), interstitial lung disease, asthma, or post-cardiac surgery.
It uses a 5-point scale (Grades 1 to 5) the higher the grade, the more severe the dyspnea (difficulty breathing).
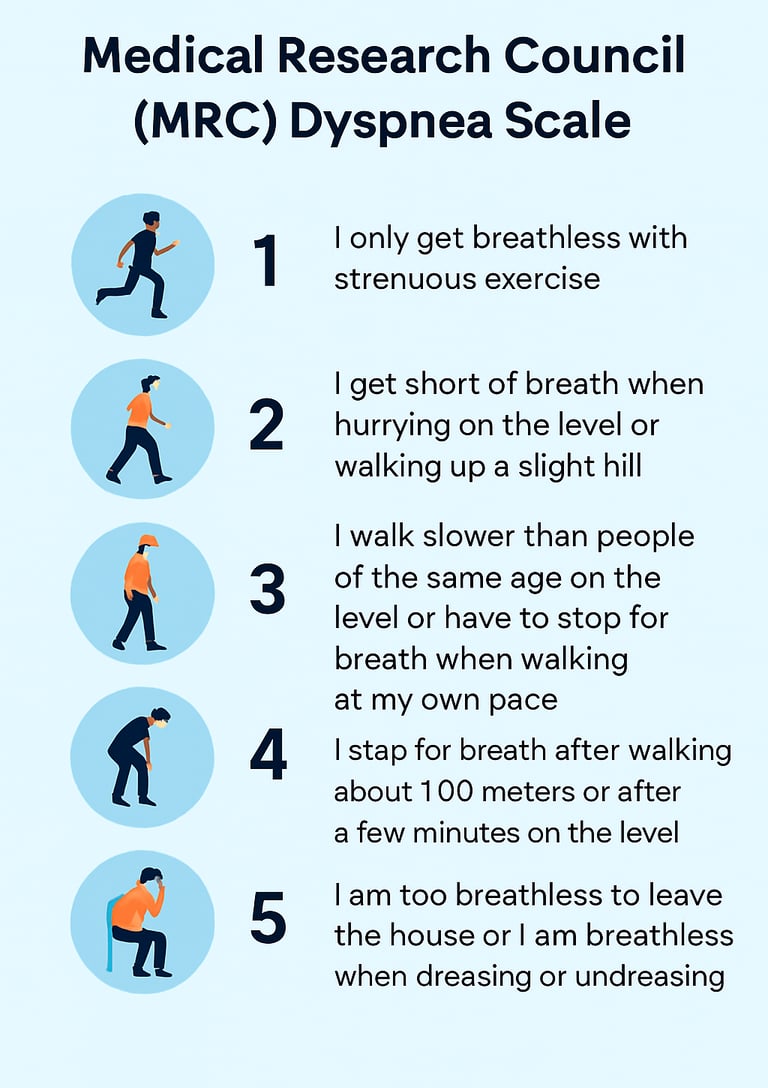
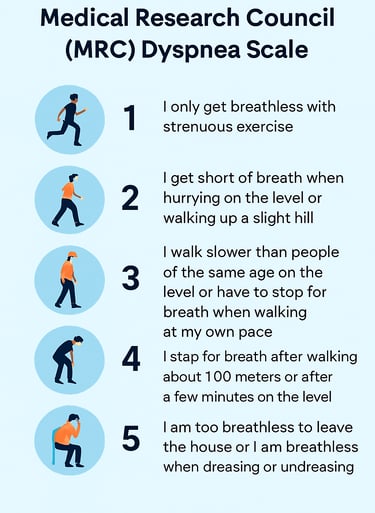
MRC Dyspnea Scale:
Grade 1 – No or minimal dyspnea
“I only get breathless with strenuous exercise.”
Patient can carry out normal activities like walking, climbing stairs, household chores without breathlessness.
Typically not restricted in lifestyle.
Often seen in early disease stages or very fit individuals.
Suggested Exercises/Advice:
Regular aerobic activity (e.g., brisk walking, cycling)
Breathing exercises like pursed-lip breathing
Maintain a healthy lifestyle
Grade 2 – Mild dyspnea
“I get short of breath when hurrying on the level or walking up a slight hill.”
May start limiting speed or avoiding hills.
Noticed in moderate activity, but still independent.
Can often still participate in most activities with mild self-pacing.
Suggested Exercises/Advice:
Interval walking: walk-rest-walk pattern
Start low-intensity pulmonary rehab
Focus on posture correction and energy conservation
Grade 3 – Moderate dyspnea
“I walk slower than people of the same age on the level because of breathlessness or have to stop for breath when walking at my own pace.”
Breathlessness affects daily living like walking, going to the market, or doing chores.
May begin avoiding social outings or outdoor activity.
Often indicative of moderate to severe lung limitation.
Suggested Exercises/Advice:
Supervised pulmonary rehabilitation
Diaphragmatic breathing training
Teach use of pacing strategies
Resistance training for limb strength
Grade 4 – Severe dyspnea
“I stop for breath after walking about 100 meters or after a few minutes on the level.”
Can walk short distances but has to pause frequently.
May need help carrying bags or doing routine chores.
Can trigger anxiety due to breathlessness.
Suggested Exercises/Advice:
Chair-based exercises
Use of walking aids with oxygen support (if prescribed)
Anxiety reduction techniques (e.g., Benson’s Relaxation, mindfulness)
Grade 5 – Very severe dyspnea
“I am too breathless to leave the house or I am breathless when dressing or undressing.”
Breathless at rest or with minimal activity.
Activities like brushing hair, dressing, or even talking can be exhausting.
May be homebound or bedbound.
Suggested Exercises/Advice:
Bed mobility and gentle limb range exercises
Positioning for breath relief (leaning forward)
Active cycle of breathing technique (ACBT)
Regular reassessment and caregiver training
Clinical Use of the MRC Scale
Quick to administer takes less than a minute.
Good screening tool for respiratory conditions.
Helps track disease progression or rehab improvement.
Often used in combination with objective measures like spirometry, 6-minute walk test, or oxygen saturation levels.
Reliability and Validity
Reliability:
The MRC scale has shown good test–retest reliability, meaning it consistently yields similar results when administered multiple times to the same individuals under similar conditions.
In a study by Bestall et al. (1999), test–retest reliability was high in patients with COPD.
Validity:
Construct Validity: The MRC scale correlates significantly with other measures of disease severity, such as: (i) FEV₁ (Forced Expiratory Volume in 1 second), (ii) 6-minute walk test (6MWT), and (iii) Health-related quality of life measures (e.g., St. George’s Respiratory Questionnaire).
Criterion Validity: MRC grades align well with clinical judgments of disability due to dyspnea. It predicts mortality and hospitalization risk in chronic respiratory disease patients.
Responsiveness: While useful for assessing baseline disability, the MRC scale is less sensitive to small changes over time compared to multi-item questionnaires like the Borg Scale or Modified Medical Research Council (mMRC) Dyspnea Scale.
References:
Paladini, L., Hodder, R., Cecchini, I., Bellia, V., & Incalzi, R. A. (2010). The MRC dyspnoea scale by telephone interview to monitor health status in elderly COPD patients. Respiratory medicine, 104(7), 1027–1034. https://doi.org/10.1016/j.rmed.2009.12.012
Bestall, J. C., Paul, E. A., Garrod, R., Garnham, R., Jones, P. W., & Wedzicha, J. A. (1999). Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax, 54(7), 581–586. https://doi.org/10.1136/thx.54.7.581
Manali, E. D., Lyberopoulos, P., Triantafillidou, C., Kolilekas, L. F., Sotiropoulou, C., Milic-Emili, J., Roussos, C., & Papiris, S. A. (2010). MRC chronic Dyspnea Scale: Relationships with cardiopulmonary exercise testing and 6-minute walk test in idiopathic pulmonary fibrosis patients: a prospective study. BMC pulmonary medicine, 10, 32. https://doi.org/10.1186/1471-2466-10-32
Nouraei, S. A., Nouraei, S. M., Randhawa, P. S., Butler, C. R., Magill, J. C., Howard, D. J., & Sandhu, G. S. (2008). Sensitivity and responsiveness of the Medical Research Council dyspnoea scale to the presence and treatment of adult laryngotracheal stenosis. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery, 33(6), 575–580. https://doi.org/10.1111/j.1749-4486.2008.01832.x
Think Anatomically. Treat Clinically.
Our Socials:
© 2025 PhysioAlchemy. All rights reserved.
Legal:
Made with ♥ by physiotherapists, for physiotherapists.
Subscribe to our newsletter:
Enjoy exclusive special deals available only to our subscribers.