Atrial Septal Defect (ASD): Causes, Symptoms, Diagnosis & Treatment
STUDY MATERIAL
PhysioAlchemy
8/2/2025
Introduction
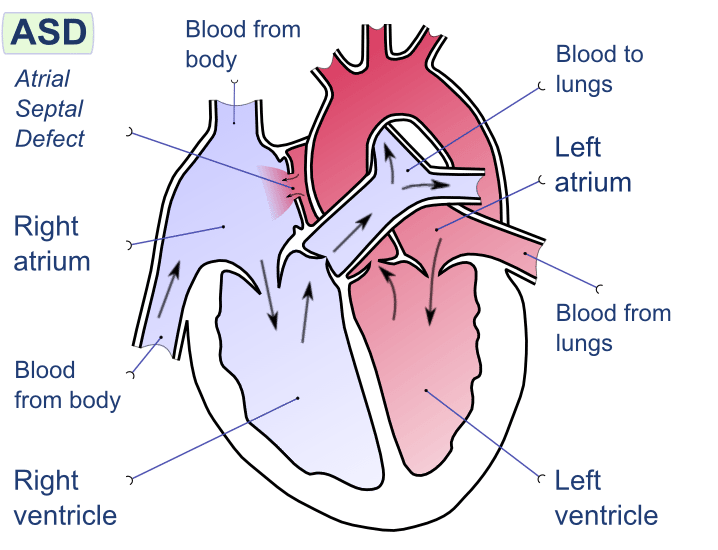
An Atrial Septal Defect (ASD) is a congenital heart condition where a hole exists in the wall (septum) that separates the two upper chambers of the heart (atria). While some ASDs are small and close on their own, larger defects can cause serious complications like pulmonary hypertension, arrhythmias, and heart failure if left untreated.
What is Atrial Septal Defect?
An Atrial Septal Defect is a type of congenital heart disease (CHD). It occurs when the septum between the left atrium and right atrium does not fully close after birth, allowing oxygen-rich blood from the left atrium to mix with oxygen-poor blood in the right atrium.
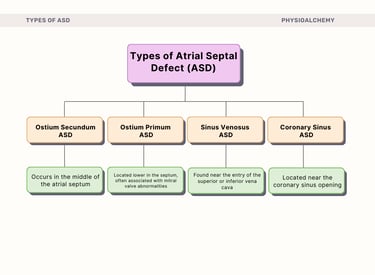
Types of ASD
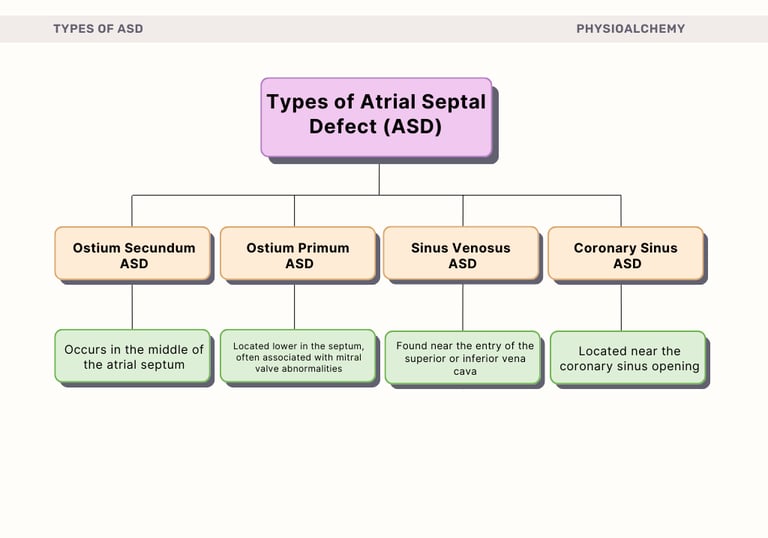
There are four main types of atrial septal defects:
Ostium Secundum ASD: (most common, ~70%): Occurs in the middle of the atrial septum.
Ostium Primum ASD: Located lower in the septum, often associated with mitral valve abnormalities.
Sinus Venosus ASD: Found near the entry of the superior or inferior vena cava.
Coronary Sinus ASD (rare): Located near the coronary sinus opening.
Causes and Risk Factors
ASD is usually present at birth (congenital). The exact cause is not always clear, but risk factors include:
Genetic factors: certain syndromes (e.g., Down syndrome).
Maternal factors: rubella infection during pregnancy, diabetes, alcohol/drug use, smoking.
Family history of congenital heart disease.
Symptoms of ASD
Many children with small ASDs are asymptomatic. Larger defects may show signs in childhood or adulthood.
Common symptoms include:
Shortness of breath, especially during exertion.
Fatigue.
Frequent respiratory infections in children.
Heart palpitations or arrhythmias.
Swelling of legs, feet, or abdomen (late stage).
Complications if Untreated
If a large ASD is left untreated, it can lead to:
Pulmonary hypertension (increased pressure in lung arteries).
Right-sided heart failure.
Arrhythmias (atrial fibrillation, flutter).
Stroke (due to paradoxical embolism).
Eisenmenger syndrome (severe pulmonary hypertension with shunt reversal).
Diagnosis
ASD can be detected using:
Echocardiogram (Echo): primary test to visualize the septal defect.
Electrocardiogram (ECG): may show arrhythmias or right heart enlargement.
Chest X-ray: enlarged heart or pulmonary arteries.
Cardiac MRI or CT scan: detailed imaging.
Cardiac catheterization: sometimes used to measure pressure changes.
Treatment Options
Treatment depends on the size, type, and symptoms of the ASD.
Observation – Small ASDs may close spontaneously in childhood.
Medications – To manage symptoms (e.g., antiarrhythmics, diuretics), but do not close the defect.
Catheter-Based Closure (Device Closure): A minimally invasive procedure using an occluder device. Best for secundum ASDs.
Surgical Repair: Open-heart surgery with sutures or a patch. Used when catheter closure is not possible.
Prognosis
Small ASDs that close naturally have an excellent outlook.
Surgical or device closure of larger ASDs has a very high success rate (>95%).
Early detection and management prevent complications and allow a normal lifespan.
Physiotherapy Management for Atrial Septal Defect (ASD) Patients
Physiotherapy plays a supportive role in patients with ASD, particularly post-surgical or post-catheter intervention, and in improving cardiorespiratory endurance, functional capacity, and quality of life.
1. Goals of Physiotherapy in ASD
The main objectives are:
Improve cardiopulmonary endurance and exercise tolerance.
Prevent post-operative complications such as atelectasis and pneumonia.
Enhance functional mobility and strength.
Educate patients on safe physical activity limits.
2. Preoperative Physiotherapy (if surgery planned)
Breathing exercises: Incentive spirometry, diaphragmatic breathing to expand lungs and reduce pulmonary complications.
Aerobic conditioning: Low-intensity walking or cycling to improve baseline endurance.
Patient education: Inform about post-op mobility and activity restrictions.
3. Postoperative Physiotherapy
Phase 1: Immediate Postoperative (0–7 days)
Respiratory exercises: Deep breathing, incentive spirometer use, coughing techniques.
Early mobilization: Bed exercises, ankle pumps, and short walks to prevent DVT.
Pain management support: Positioning and gentle movement to reduce discomfort.
Phase 2: Early Recovery (1–6 weeks)
Gradual ambulation: Increase walking distance progressively.
Gentle aerobic activity: Stationary bike or light treadmill sessions.
Stretching & flexibility: Upper and lower limb stretches to maintain joint mobility.
Phase 3: Late Recovery (6 weeks–3 months)
Cardiorespiratory endurance: Moderate-intensity exercises, guided by heart rate and tolerance.
Strengthening exercises: Light resistance training focusing on large muscle groups.
Functional activities: Stair climbing, household tasks, and recreational activities.
Precautions:
Avoid strenuous activity if significant residual shunt, pulmonary hypertension, or arrhythmias exist.
Monitor heart rate, oxygen saturation, and signs of fatigue.
Collaborate with cardiologist for exercise prescription.
4. Pediatric Considerations
Encourage play-based aerobic activities (cycling, swimming, running in controlled settings).
Avoid high-contact sports if unrepaired ASD exists.
Monitor growth and development, as chronic large ASDs can lead to delayed growth.


References:
Menillo AM, Alahmadi MH, Pearson-Shaver AL. Atrial Septal Defect. [Updated 2025 Jan 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535440/
Rakhmawati A, Achmad IN, Hartopo AB, Anggrahini DW, Arso IA, Emoto N, Dinarti LK. Exercise Program Improves Functional Capacity and Quality of Life in Uncorrected Atrial Septal Defect-Associated Pulmonary Arterial Hypertension: A Randomized-Control Pilot Study. Ann Rehabil Med. 2020 Dec;44(6):468-480. doi: 10.5535/arm.20100. Epub 2020 Dec 31. PMID: 33440095; PMCID: PMC7808796.
Tsuda T, Davies RR, Radtke W, Pizarro C, Bhat AM. Early Surgical Closure of Atrial Septal Defect Improves Clinical Status of Symptomatic Young Children with Underlying Pulmonary Abnormalities. Pediatr Cardiol. 2020 Aug;41(6):1115-1124. doi: 10.1007/s00246-020-02361-8. Epub 2020 May 9. PMID: 32388668; PMCID: PMC7223328.
Langeveld YF, Ter Hoeve N, van den Bosch A, Robbers-Visser D, Kauling RM, van Groen JC, Sunamura M, Jorstad HT, Snaterse M. Physical exercise barriers and needs in adults with congenital heart disease: a qualitative study. BMJ Open. 2025 Jul 5;15(7):e102090. doi: 10.1136/bmjopen-2025-102090. PMID: 40617613; PMCID: PMC12228472.
Barth J, Dewald O, Ewert P, Freiberger A, Freilinger S, Gampert T, Harig F, Hörer J, Holdenrieder S, Huntgeburth M, Kaemmerer-Suleiman AS, Kohls N, Nagdyman N, Neidenbach R, Schmiedeberg W, Suleiman MN, von Scheidt F, Koch D, Wagener W, Mentzner D, Kaemmerer H, Mellert F. Cardiological rehabilitation, prehabilitation, and cardiovascular prevention in adults with congenital heart defects: tasks and services of the German Pension Insurance-part 1: preventive cardiology and prehabilitation. Cardiovasc Diagn Ther. 2025 Jun 30;15(3):684-695. doi: 10.21037/cdt-2024-691. Epub 2025 Jun 26. PMID: 40656789; PMCID: PMC12246989.
Think Anatomically. Treat Clinically.
Our Socials:
© 2025 PhysioAlchemy. All rights reserved.
Legal:
Made with ♥ by physiotherapists, for physiotherapists.
Subscribe to our newsletter:
Enjoy exclusive special deals available only to our subscribers.